Candida
CASE 1
• A 10 month old boy is brought to the physician because of a irritable rash over the pubic area, bilateral inguinal areas and perineum. The rash involves the penis and scrotum as well as the adjacent thigh skin. It has well-defined margins, but there are "satellite" lesions that are separated from the main, continguous rash. The child has no fever and does not appear ill.

• The mother is given nystatin powder to use on the rash, both the kill the fungus and to keep the area dry. The
Questions:
1. If you wished to confirm the presence of candida infection causing this rash, how would you isolate the infecting strain in the laboratory?
2. What will Candida albicans look like when it is growing on an agar plate?
3. What will the organisms from the culture look like on a Gram stain? How does this differ from their appearance in human tissues?
4. Where did the C. albicans come from that caused this rash? From the baby? The mother? The environment?
5. Why did the baby develop this infection? What are the consequences of not treating it?
6. Does the presence of this infection in this child suggest that the has an underlying disease?
CASE 2
• An 18 year old woman has vaginal itching and a discharge that looks like "toothpaste" for the past 2 days. She has never had a similar discharge in the past. Six days ago, she completed a course of an antibiotic for a "sinus infection," which has now resolved completely.
• A pelvic examination revealed a thick white discharge on the vaginal wall and cervix (below).
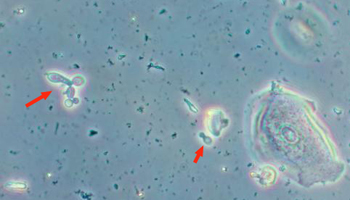
• Some of the white material was adherent to the vaginal wall but could be scraped off with a tongue depressor. A wet mount of the discharge confirmed the presence of budding yeast (red arrow, lower right) and a cluster of yeast beginning to extend pseudohyphae (red arrow, left).
• The patient was treated with miconazole vaginal inserts and promptly recovered.
Questions:
1. Is this a sexually-transmitted disease? If not, from where did the Candida in this patient's vagina arise?
2. Why did Candida begin to grow to excess in the vagina?
3. What was the role of her antibiotic therapy in the development of this vaginitis? What was the role of normal vaginal flora in this scenario?
4. What other clinical situations are associated with vaginal candidiasis?
5. What local tissue conditions are optimal for the overgrowth of Candida?
CASE 3
• A 30 year old divorced man presents with cough, fever, and chest pain of two weeks duration. He also reports soreness in his mouth and pain with swallowing for the past 6 weeks. He believes that he is losing weight because his clothes are becoming looser, but he does not have a scale. He has not taken any antibiotics.
• On examination, there are crackles heard over the entire right lung and dullness to percussion at the right base. Examinatnion of the mouth shows the following findings:
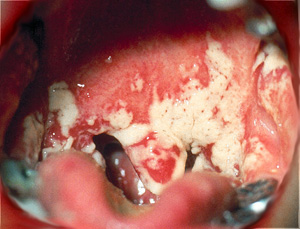
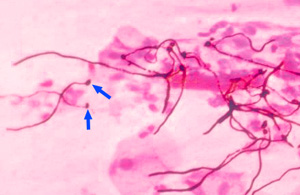
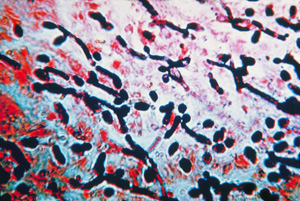
• The white plaque on his palate and buccal mucosa can be scraped off. A sample is smeared on a slide and Gram stained. Several pseudohyphae are seen, arising from oval-shaped, yeast cells (which usually stain Gram-positive). Note that the yeast and pseudohyphae are much larger than bacteria, which cannot be visualised at this magnification.
 .
.
• A chest xray confirms the presence of a right upper lobe cavitating infiltrate and a right pleural effusion. This finding and the presence of oral thrush (candidiasis) raise a strong suspicion for tuberculosis in the setting of HIV/AIDS. An HIV test is ordered and is positive.
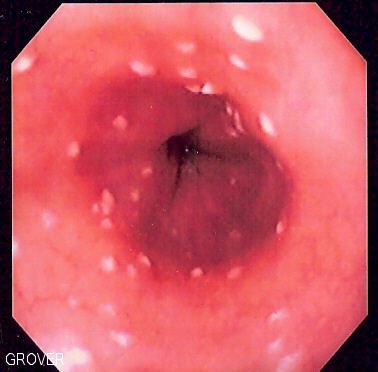
• Because of the difficulty swallowing, the patient undergoes endoscopy to visualize his esophagus. The examination reveals white plaques along the entire extent of the esophagus (left). A biopsy is taken, and a tissue Gram stain shows budding yeast and yeast forming pseudohyphae (right).
Questions:
1. What is the significance of oral thrush (candidiasis) in an adult patient?
2. When candida overgrows in a patient with HIV/AIDS, where would you expect to find it? Is it common for candida to invade the bloodstream in AIDS patients? If not, what other category of patients may dissseminate candida in the bloodstream? Why is there a difference?
3. Should all HIV patients be put on continuous therapy to suppress candida (e.g., with daily fluconazole)? What would be the potential downside of doing this routinely?
4. How should this patient be treated for his candida esophagitis?